As we age, our bodies face new challenges, and one common issue many seniors encounter is toenail fungus. If you’ve been battling this persistent problem, you might be wondering: how can I tell if the treatment is working? How do I know if my toenail fungus is dying? As a dermatologist with over two decades of experience specializing in nail health, I’m here to guide you through the signs that indicate your toenail fungus may be on its way out.
Understanding Toenail Fungus in Seniors
Before we dive into the signs of dying toenail fungus, let’s briefly discuss why this condition is particularly prevalent among seniors. As we age, several factors increase our risk of developing toenail fungus. Our nails grow more slowly, and the reduced blood circulation in our feet can make it harder for our bodies to fight off infections. Additionally, our immune systems may not be as robust as they once were, making us more susceptible to fungal invasions.
Years of accumulated exposure to fungi also play a role. Think about all the public pools, locker rooms, and shared spaces we’ve walked through barefoot over the decades. Each of these instances presented an opportunity for fungi to take hold. Lastly, as we age, maintaining proper foot hygiene can become more challenging due to reduced flexibility, making it harder to reach and care for our toes effectively.
Types of Nail Fungus
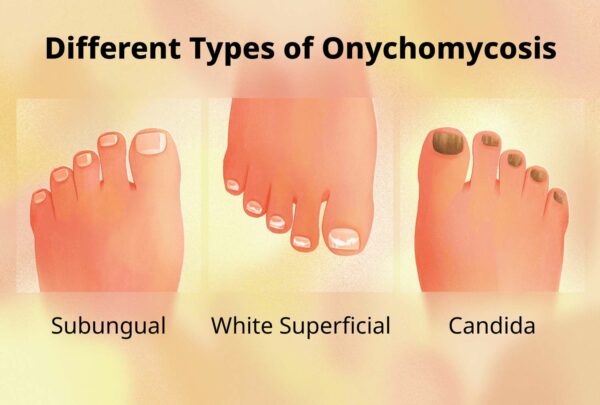
There are several types of toenail fungus, each caused by different organisms. Understanding which type you have can help in determining the most effective treatment. The main types include:
- Distal Subungual Onychomycosis (DSO): This is the most common type, affecting the nail bed and underside of the nail plate. It’s caused by the same fungus that causes athlete’s foot.
- White Superficial Onychomycosis (WSO): This type affects the surface of the nail plate and appears as white spots on the toenail.
- Proximal Subungual Onychomycosis (PSO): Less common, this type starts at the base of the nail and moves outward. It’s more prevalent in people with weakened immune systems.
- Candidal Onychomycosis: This is caused by Candida yeast and often affects fingernails more than toenails.
- Total Dystrophic Onychomycosis: This is the most severe form, where the entire nail plate is affected and can be the end stage of any of the other types.
For seniors, DSO is the most common type we encounter in our practice. However, regardless of the type, the signs of improvement and the treatment process are similar.
Stages of Toenail Fungus Progression
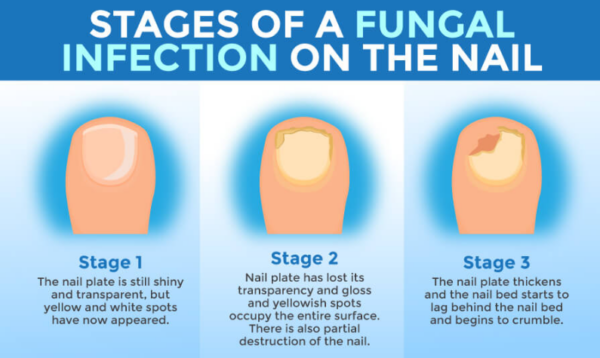
Understanding the stages of toenail fungus can help you recognize improvement. Generally, toenail fungus progresses through three stages:
- Early Stage: The fungus has just begun to take hold. You might notice a white or yellow spot under the tip of your toenail. The nail might be slightly thickened or discolored.
- Intermediate Stage: The fungal infection has spread deeper into the nail. The nail becomes more discolored (often yellow or brown), thickens, and may become brittle. You might notice debris under the nail.
- Advanced Stage: The nail is severely discolored, thickened, and misshapen. It may separate from the nail bed (a condition called onycholysis) and become painful. The infection might spread to other toes or even your skin.
Recognizing these stages can help you understand how far your infection has progressed and how to gauge improvement.
Signs That Your Toenail Fungus Is Dying

Now, let’s address the main question: how can you tell if your toenail fungus is dying? Here are the key indicators to look out for:
1. Changes in Nail Color
One of the first signs that your toenail fungus is dying is a change in the color of your affected nail. When you first develop a fungal infection, your nail often appears yellow, brown, or even greenish. These discolorations are caused by the fungi metabolizing your nail tissue and the debris they leave behind.
As the fungus begins to die off, you’ll notice your nail starting to return to its natural color. This process typically begins at the base of the nail, where new, healthy nail growth originates. You might observe a distinct line between the healthy and infected parts of your nail as the clear, uninfected nail grows in. Remember, this process is gradual and can take several months to become noticeable, so patience is key.
2. Improved Nail Texture
Fungal infections often cause nails to become thick, brittle, and crumbly. This change in texture occurs because the fungi feed on the keratin in your nails, weakening their structure. As the fungus dies and your nail begins to heal, you’ll notice improvements in its texture.
The nail will gradually become less thick and less brittle. You might find that your nail doesn’t break or chip as easily as it did when it was infected. The surface of the nail may become smoother, losing that rough, uneven appearance characteristic of fungal infections. This change in texture is a positive sign, indicating that new, healthy nail is growing and replacing the damaged tissue.
3. Reduced Nail Thickening
Toenail fungus often causes the nail to thicken significantly, a condition known as onychauxis. This thickening occurs as your body tries to protect itself from the infection by producing more nail tissue. As the fungus dies off and your treatment takes effect, you may notice the nail becoming thinner.
This reduction in thickness is a gradual process and may take several months to become noticeable. You might find that it becomes easier to trim your nails, and your shoes might feel more comfortable as the thickened nail no longer presses against them. However, it’s important to note that some residual thickening may persist even after the infection clears, especially in older individuals where age-related thickening is common.
4. New Nail Growth
Perhaps the most encouraging sign of dying toenail fungus is the appearance of new, healthy nail growth. Look for clear, uninfected nail growing from the base of your nail bed. This new growth will slowly push out the infected part of the nail.
It’s important to understand that this process takes time, especially for seniors. Toenails grow slowly, at an average rate of about 1.6 mm per month. This means it can take 12-18 months for a toenail to be completely replaced. The new growth will appear smoother and have a more normal color compared to the infected portion of the nail.
As the new nail grows, you might notice a distinct line separating the healthy new growth from the old, infected nail. This line will gradually move towards the tip of your toe as the new nail pushes out the old.
5. Reduced Nail Separation
In severe fungal infections, the nail may separate from the nail bed, a condition known as onycholysis. This separation occurs because the infection weakens the connection between the nail plate and the nail bed. As the fungus dies and your nail begins to heal, you may notice the nail starting to reattach to the nail bed.
The white or yellow separation at the tip or sides of the nail may decrease. This reattachment is a slow process but a very positive sign of healing. It indicates that the nail bed is recovering and new, healthy nail is growing attached to it.
6. Decreased Nail Debris
Fungal infections often cause a buildup of debris under the nail. This debris consists of dead skin cells, bits of infected nail, and fungal matter. As the fungus dies off, you may notice less debris accumulating under the nail.
The nail may appear cleaner overall, with less of the chalky or flaky substance that often accompanies fungal infections. This reduction in debris is a good indicator that the fungal infection is losing its hold and your nail is returning to a healthier state.
The Importance of Patience in Toenail Fungus Treatment
It’s crucial to understand that seeing signs of improvement doesn’t mean the treatment is complete. Toenail fungus is notoriously persistent, and treatment must be continued even after symptoms improve. Full regrowth of a healthy nail can take 12-18 months, given the slow growth rate of toenails, especially in seniors.
Consistency is key in treating toenail fungus. Continue your treatment as prescribed, even if you see improvement. Stopping treatment too soon can lead to a recurrence of the infection, potentially undoing months of progress. Regular check-ups with your healthcare provider are essential to monitor your progress and adjust the treatment plan if necessary. Check our article to know all the toenail fungus cure options available.
Treatment Options for Toenail Fungus
There are several treatment options available for toenail fungus, ranging from over-the-counter solutions to prescription medications. The choice of treatment often depends on the severity of the infection and your overall health status.
Over-the-Counter (OTC) Treatments

OTC antifungal nail creams and ointments are available and can be effective, depending on their formula. Regularly they contain ingredients like clotrimazole, terbinafine, or undecylenic acid. While these can be a good starting point, they may not be strong enough for more severe infections.
Many of my patients have seen very promising results with topical treatments like the Swissklip Anti-Fungal Stick, which can be an effective part of a comprehensive toenail fungus treatment plan when used consistently. Its easy-to-use applicator makes it particularly suitable for seniors who may have difficulty applying creams or ointments.
Prescription Medications
If you’d prefer to go with prescribed medications, your doctor may prescribe oral antifungal medications. The most common are:
- Terbinafine (Lamisil): This is often the first choice due to its effectiveness. Studies show a cure rate of about 70% after 12 weeks of treatment.
- Itraconazole (Sporanox): Another effective option, with cure rates similar to terbinafine.
- Fluconazole (Diflucan): While less commonly used for nail infections, it can be effective in some cases.
These medications typically need to be taken for 6 to 12 weeks. It’s important to note that while they’re effective, they can have side effects and may interact with other medications. Always consult with your healthcare provider before starting any new treatment.
Topical Prescription Medications
There are also prescription-strength topical treatments available, such as:
- Ciclopirox (Penlac): This is applied to the infected nails and surrounding skin daily.
- Efinaconazole (Jublia): A newer topical treatment that has shown good efficacy in clinical trials.
These topical treatments generally have fewer side effects than oral medications but may take longer to show results.
When to Seek Professional Help

While it’s encouraging to see signs of improvement, there are times when you should consult a healthcare professional:
- If you have diabetes or circulatory issues: These conditions can complicate foot health and increase the risk of serious infections.
- If the infection appears to be spreading: If you notice the fungus affecting more nails or the surrounding skin, it’s time to see a doctor.
- If you experience pain or discomfort: Fungal infections shouldn’t typically cause pain. If you’re experiencing discomfort, there might be a secondary bacterial infection or another issue.
- If you see no improvement after several months of treatment: Sometimes, what appears to be a fungal infection might be another condition, or the fungus might be resistant to your current treatment.
- If you have a weakened immune system: Conditions that affect your immune system can make fungal infections more serious and harder to treat.
As a senior, it’s especially important to seek professional help for foot-related issues to prevent complications. Don’t hesitate to reach out to a podiatrist or dermatologist if you have any concerns about your toenail fungus treatment.
Special Considerations for Seniors

As we age, there are some additional factors to consider when dealing with toenail fungus:
- Reduced Circulation: Poor circulation can slow healing. Regular exercise, even gentle activities like walking, can help improve blood flow to your feet.
- Weakened Immune System: A less robust immune system can make infections harder to fight. Eating a balanced diet rich in vitamins and minerals can help support your immune function.
- Difficulty with Foot Care: If you find it challenging to care for your feet due to reduced flexibility or vision problems, consider asking for help from a family member or professional pedicurist who specializes in senior foot care.
- Medication Interactions: If you’re on multiple medications, be sure to inform your doctor before starting any new treatments for toenail fungus, as there could be potential interactions.
- Slower Nail Growth: As nail growth slows with age, it may take longer to see results from treatment. Patience and consistency are key.
Increased Risk of Complications: Due to factors like reduced sensation in the feet and slower healing, seniors are at higher risk for complications from toenail fungus. Regular check-ups with a podiatrist or dermatologist are important.
Frequently Asked Questions
To address some common concerns seniors might have about toenail fungus, here are answers to frequently asked questions:
Q1: How long does it take to see signs of improvement in toenail fungus?
A: The timeline for improvement can vary, but most people start to see some positive changes within a few months of consistent treatment. However, complete resolution can take 9-12 months or longer, especially for seniors whose nails grow more slowly. Remember, the key is to be patient and consistent with your treatment.
Q2: Can toenail fungus go away on its own?
A: It’s rare for toenail fungus to resolve without treatment, especially in seniors. Our immune systems become less efficient as we age, making it harder for our bodies to fight off infections on their own. Without treatment, the infection usually worsens over time, potentially spreading to other nails or causing more severe complications.
Q3: Is it normal for the nail to fall off during treatment?
A: In some cases, the infected nail may loosen and fall off during treatment. While this might seem alarming, it’s not necessarily a bad thing. When the infected nail falls off, it allows a new, healthy nail to grow in its place. This process can actually speed up your recovery, as the new nail growth is typically free from infection.
Q4: Can I use nail polish while treating toenail fungus?
A: It’s generally best to avoid nail polish during treatment for toenail fungus. Nail polish can trap moisture against your nail, potentially creating an environment where fungi can thrive. Additionally, some treatments need to penetrate the nail to be effective, and nail polish can interfere with this process. If you feel you must use polish for cosmetic reasons, opt for antifungal nail polishes, but discuss this with your healthcare provider first.
Q5: Are there any natural remedies that can help with toenail fungus?
A: Some people find success with natural remedies like tea tree oil, apple cider vinegar, or oregano oil. These substances have antifungal properties that may help combat the infection. However, it’s important to note that while these natural remedies might be helpful for mild cases or as a complementary treatment, they should not replace prescribed treatments, especially for more severe or persistent infections. Always discuss any natural remedies you’re considering with your healthcare provider to ensure they won’t interact with your other treatments or health conditions.
Q6: Can I spread toenail fungus to other people?
A: Yes, toenail fungus can be contagious. It can spread to other people through direct contact or by sharing items like towels, nail clippers, or shoes. This is why it’s important to take precautions, such as wearing shower shoes in public areas and not sharing personal care items, even with family members.
Q7: Will my toenails ever look completely normal again?
A: In many cases, with proper treatment and care, your toenails can return to a normal or near-normal appearance. However, it’s important to have realistic expectations. Some people, especially seniors, may have some residual nail changes even after the fungus is gone due to age-related changes in the nail or damage from the long-term infection. The goal of treatment is to eliminate the fungus and improve the nail’s appearance and health, even if it doesn’t return to exactly how it looked before the infection.
Q8: How can I prevent toenail fungus if I have diabetes?
A: If you have diabetes, you’re at higher risk for toenail fungus and its complications. To prevent infection:
- Keep your blood sugar levels well-controlled
- Inspect your feet daily for any changes or injuries
- Keep your feet clean and dry
- Wear diabetic socks that wick away moisture
- See a podiatrist regularly for professional foot care
- Use antifungal sprays or powders in your shoes
- Consider using a product like the Swissklip Anti-Fungal Stick as a preventive measure
Remember, any foot-related issues should be taken seriously if you have diabetes. Consult your healthcare provider promptly if you notice any changes in your toenails or feet.
Final Thoughts

Dealing with toenail fungus can be a long and sometimes frustrating process, especially for seniors. However, with the right treatment, consistent care, and a bit of patience, you can overcome this common condition. By understanding the signs of improvement and knowing when to seek professional help, you’re well-equipped to tackle toenail fungus effectively.
Remember, healthy feet play a crucial role in maintaining your overall quality of life, enabling you to stay active and independent. Don’t hesitate to reach out to healthcare professionals for guidance and support throughout your treatment journey. With perseverance and proper care, you can look forward to healthier, clearer nails and improved foot health.
Dr. Mark Griffin is a board-certified dermatologist with over 20 years of experience specializing in nail health. He is the author of bestselling books on nail care and runs a popular blog dedicated to helping people achieve optimal nail health.
How We Reviewed This Article
SOURCES This article is based on scientific studies, expert opinions, and reputable health organizations. Key sources include:
- Sudhir Baswan, et al. (2017). Understanding the Formidable Nail Barrier: A Review of the Nail Microstructure, Composition and Diseases. PudMed Central. DOI: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5383514/
- Eisman Samantha and Sinclair Rodney. (2014). Fungal nail infection: diagnosis and management. British Medical Journal. PMID: 24661991 DOI: https://www.bmj.com/content/348/bmj.g1800
- Institute for Quality and Efficiency in Health care. Cologne, Germany. Nail fungus: Learn More – Nail fungus: Polish, cream or tablets? https://www.ncbi.nlm.nih.gov/books/NBK279546/
- Angelo Tamara, et al. (2017). Chemical and physical strategies in onychomycosis topical treatment: A review. Medical Mycology, Volume 55, Issue 5, July 2017, Pages 461–475, https://doi.org/10.1093/mmy/myw084
HISTORY This article was written by Dr. Mark Griffin, reviewed by our medical team, and published on July 25, 2024. We regularly update our content to reflect new research and ensure its accuracy and relevance.