As we age, our nails can sometimes give us a bit of trouble, and it’s not always easy to tell what’s causing the issue.
Today, we’re going to talk about two common conditions that often confuse my patients: nail psoriasis and fungal infections.
You know, in my 20 years as a dermatologist, I’ve seen countless patients struggling to distinguish between these two conditions. It’s a common dilemma, especially for seniors. Did you know that more than 3% of the US adult population is affected by psoriasis? That’s more than 7.5 million US adults. Also, up to 50% of people with psoriasis experience nail changes? And nail fungus? It affects about 10% of the general population, but that number jumps to nearly 50% in people over 70!
Understanding the difference between nail psoriasis and fungus is crucial for proper treatment. So, let’s dive in and demystify these conditions together, shall we?
Understanding Nail Psoriasis

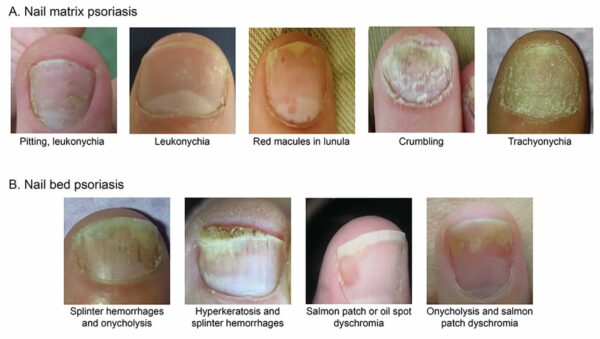
First, let’s talk about nail psoriasis. This isn’t just a nail problem – it’s actually a manifestation of psoriasis, an autoimmune condition that affects the skin. In nail psoriasis, the nail growth process is disrupted, leading to various changes in the nail’s appearance and structure.
What causes nail psoriasis, you ask? Well, like other forms of psoriasis, it’s believed to be the result of an overactive immune system. Your body essentially attacks its own tissues, including the nail unit. Genetics play a role too – if you have a family history of psoriasis, you’re at higher risk.
Now, what does nail psoriasis look like? It can vary, but common signs include:
- Pitting: Small depressions on the nail surface, like someone took a tiny ice pick to your nail.
- Onycholysis: The nail separates from the nail bed, often starting at the tip and working its way back.
- Oil drop or salmon patch: A reddish-orange discoloration visible through the nail.
- Subungual hyperkeratosis: A chalky buildup under the nail.
You might also notice that your nails become thick, brittle, or change color. Some of my patients describe their nails as looking “crumbly” or “ragged.”
Demistifying Nail Fungus

Now, let’s switch gears and talk about nail fungus, or onychomycosis as we call it in medical terms. This is a common infection caused by various types of fungi, including dermatophytes, yeasts, and molds.
Fungal infections love warm, moist environments – that’s why they often start in toenails. Risk factors include aging (our immune systems aren’t as robust as they used to be), poor circulation, and diabetes. Even something as simple as walking barefoot in public areas like locker rooms can increase your risk.
So, what does nail fungus look like? Common signs include:
- Thickening of the nail
- Discoloration (often yellow or brown)
- Brittleness or crumbling edges
- A slightly foul odor
You might also notice white or yellow patches on the nail surface, or even a chalky white buildup of dead cells under the nail, not unlike what we see in nail psoriasis.
Key Differences Between Nail Psoriasis vs Fungus

Now, I know what you’re thinking – these conditions sound pretty similar! And you’re right, they can be tricky to tell apart. But there are some key differences:
- Distribution: Nail psoriasis often affects several nails at once and might be accompanied by skin symptoms elsewhere on the body. Fungal infections typically start with one nail and spread gradually.
- Pitting: Those little dents I mentioned earlier? They’re a hallmark of psoriasis and rarely seen in fungal infections.
- Nail separation: While both conditions can cause the nail to lift from the nail bed, in psoriasis, it often starts at the tip and moves backward. In fungal infections, it usually begins at the sides or base.
- Associated symptoms: Psoriasis might cause pain or tenderness around the nail, while fungal infections are usually painless unless they become severe.
- Progression: Nail psoriasis tends to develop quickly and affect multiple nails simultaneously. Fungal infections usually progress slowly, often starting with a single nail.
Diagnostic Process
Now, how do we figure out which condition you’re dealing with? It starts with a thorough examination and medical history. Usually, doctors have to ask about your symptoms, when they started, and any other health conditions you might have.
For nail psoriasis, we might perform a biopsy if the diagnosis isn’t clear. This involves taking a small sample of the nail or surrounding skin for analysis.
For fungal infections, we often use what’s called a KOH test. We’ll take some debris from under your nail and examine it under a microscope. In some cases, we might do a fungal culture to identify the specific type of fungus.
Treatment Options:
Once we’ve nailed down the diagnosis (pun intended!), we can talk about treatment.
For nail psoriasis, we have several options:
- Topical treatments: Corticosteroids, vitamin D analogs, or retinoids can be applied directly to the nail and surrounding skin.
- Systemic medications: For severe cases, oral medications that affect the immune system might be necessary.
- Light therapy: Exposing the nails to specific wavelengths of light can help in some cases.
For fungal infections, we typically use:
- Topical antifungal solutions: These are applied directly to the nail and surrounding skin. A great option I always recommend is the Swissklip Antifungal Stick, a fungus treatment that restores the discolored appearance of damaged nails.
- Oral antifungal medications: For more stubborn infections, oral medications might be necessary.
- Nail removal: In severe cases, we might need to remove the infected nail to treat the nail bed directly.
In both cases, patience is key. Nails grow slowly, especially as we age, so it can take several months to see improvement.
Prevention Strategies

Of course, prevention is always better than cure. Here are some tips to keep your nails healthy:
- Keep your nails clean and dry.
- Wear breathable footwear and change your socks daily.
- Don’t go barefoot in public areas like locker rooms or swimming pools.
- Manage underlying health conditions like diabetes.
- Eat a balanced diet rich in vitamins and minerals that support nail health.
When to Seek Professional Help:
If you notice any changes in your nails – discoloration, thickening, separation from the nail bed, or anything else that seems off – it’s best to get it checked out. Early intervention can make a big difference in treatment outcomes.
Living with Nail Conditions: Tips for Seniors
I know dealing with nail conditions can be frustrating, especially if they affect your daily activities. Some of my patients find it helpful to:
- Use special thick nail clippers designed for problem nails.
- Soak nails before trimming with Swissklip Heavy Duty toenail clipper, to soften them. Read our article to know how to cut thick toenails.
- Wear comfortable, roomy shoes to reduce pressure on affected nails.
- Be patient and kind to yourself – healing takes time.
FAQs About Nail Psoriasis and Fungus
Q: Can I have both nail psoriasis and a fungal infection? A: Yes, it’s possible to have both conditions simultaneously, which is why professional diagnosis is so important.
Q: Will my nails ever look normal again? A: With proper treatment, many people see significant improvement. However, some changes might be permanent, especially if the condition has been present for a long time.
Q: Are these conditions contagious? A: Nail psoriasis is not contagious. Fungal infections can be spread, but typically require direct contact.
Q: Can diet affect my nail health? A: Yes, a balanced diet rich in vitamins and minerals can support overall nail health. Some studies suggest that certain dietary changes might help manage psoriasis symptoms.
Conclusion
Remember, whether you’re dealing with nail psoriasis, a fungal infection, or something else entirely, you don’t have to face it alone. With proper diagnosis and treatment, we can work together to improve the health of your nails and your overall quality of life.
If you’re noticing changes in your nails, don’t hesitate to reach out to a dermatologist or podiatrist. Early intervention can make a world of difference.
Take care of those nails, and they’ll continue to serve you well for years to come!
Dr. Mark Griffin is a board-certified dermatologist with over 20 years of experience specializing in nail health. She is the author of bestselling books on nail care and runs a popular blog dedicated to helping people achieve optimal nail health.
How We Reviewed This Article
SOURCES This article is based on scientific studies, expert opinions, and reputable health organizations. Key sources include:
- Armstrong, et al. (2021). About Psoriasis. National Psoriasis foundation. DOI: https://www.psoriasis.org/about-psoriasis/
- American Academy of Dermatology Association. Nail fungus: Diagnosis and treatment. https://www.aad.org/public/diseases/a-z/nail-fungus-treatment
- The Psoriasis and Psoriatic Arthritis Alliance. Psoriasis in the nails. 2024 https://www.papaa.org/learn-about-psoriasis-and-psoriatic-arthritis/psoriatic-disease-unlocked/nail-psoriasis/
- Scher, Richard K (1995). Psoriasis of the Nails. DOI: https://www.nailsmag.com/392363/psoriasis-of-the-nails
HISTORY This article was written by Dr. Mark Griffin, reviewed by our medical team, and published on July 25, 2024. We regularly update our content to reflect new research and ensure its accuracy and relevance.